Clinicians continue to face several challenges related to Clinical Communication & Collaboration (CC&C), even as adoption of digital tools accelerates. These issues often stem from fragmentation, workflow misalignment, and legacy infrastructure. Here are the key points:
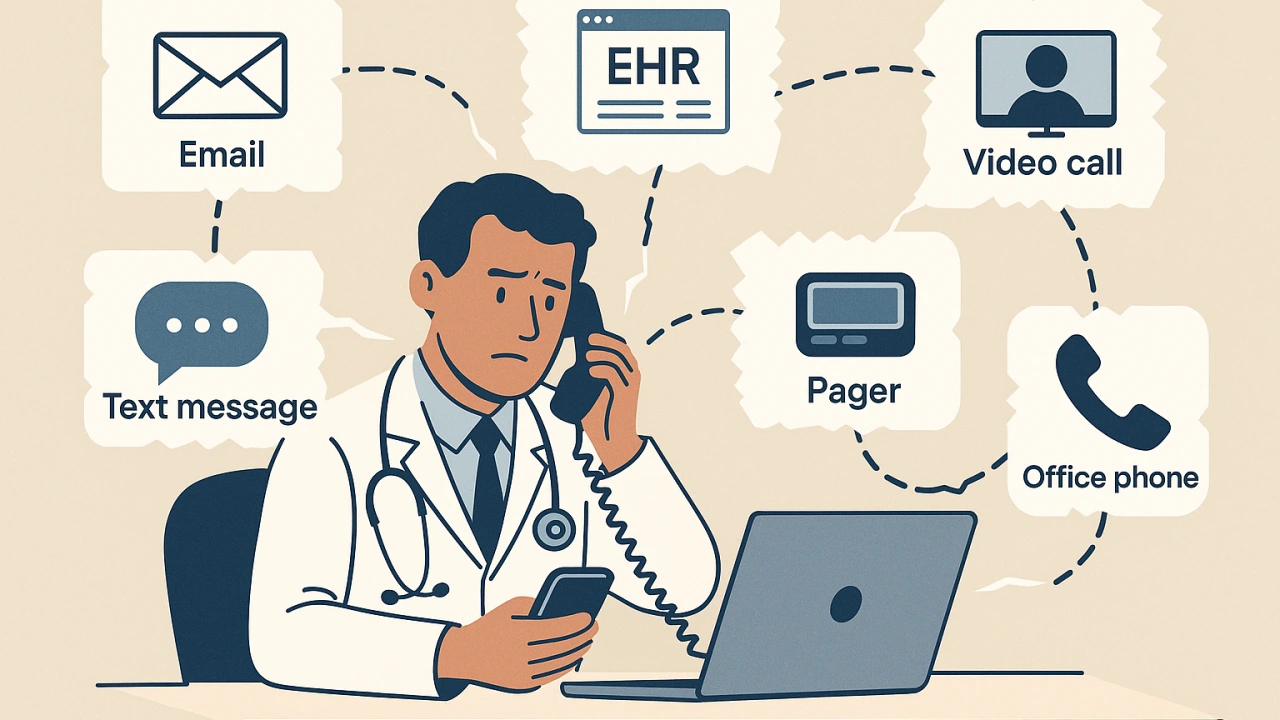
Fragmented Communication Channels
Clinicians often use patchwork tools—EHR messaging, email, phones, pagers, and third-party apps—that don’t integrate well.
- Problem: Information is scattered across platforms, leading to delayed responses, missed messages, and duplication.
- Example: A nurse sends a message through the EHR, but the on-call physician receives critical updates via a separate mobile app.
Lack of Real-Time, Role-Based Routing
Many systems don’t account for clinical roles and shift schedules, leading to misrouted alerts and wasted time identifying the right contact.
Impact: Nurses or physicians must manually locate the correct on-call colleague, increasing care delays and clinician frustration.
Alert Fatigue and Interruptions
CC&C platforms often generate high volumes of non-urgent alerts without adequate filtering or prioritization.
Consequence: Increased risk to patient safety and elevated cognitive load.
Result: Clinicians become desensitized, sometimes ignoring true high-priority messages.
Poor EHR Integration
Many CC&C tools lack seamless integration with EHRs, resulting in:
- Manual data entry,
- Inability to view patient context during messaging,
- Fragmented documentation trails. This breaks clinical workflows and reduces the overall utility of communication systems.
Device Overload
Providers may carry multiple devices: hospital-issued smartphones, personal phones, tablets, and pagers.
- Problem: Juggling between them causes inefficiencies and confusion, especially during emergencies.
Security and Compliance Barriers
Strict HIPAA rules require secure messaging, authentication, and audit logging.
- Many clinicians still resort to unsecured texting due to ease of use, putting PHI at risk.
- Workarounds indicate poor user experience in officially approved CC&C apps.
Resistance to Workflow Change
Adoption of CC&C tools requires workflow redesign.
- Clinicians often resist changes due to steep learning curves, loss of efficiency, or perceived additional burden.
- Leadership may not fully engage frontline users during selection or rollout, compounding the problem.
Lack of Standardization Across Facilities
Different departments may use various communication platforms, especially in health systems with multiple hospitals or practices, complicating cross-team collaboration and continuity of care.
Limited Patient Engagement Integration
Most CC&C systems focus on clinician-to-clinician communication. However, there’s a growing demand for bidirectional communication with patients (especially for post-acute care, discharge instructions, and remote monitoring).
- Current tools lack integration with patient apps or portals, limiting holistic care coordination.
Emerging Technologies and Trends in Clinical Communication and Collaboration (CC&C) Industry
- Telehealth & Multi-Channel Communication: The pandemic has accelerated telemedicine, integrating video and remote collaboration into CC&C platforms. Modern systems support real-time conferencing (e.g., tele-ICU) alongside messaging and voice, allowing care teams to communicate “anywhere, anytime.”
- EHR Integration & Contextual Workflows: Next-gen CC&C tools extract data from EHRs and hospital systems to streamline workflows. They integrate clinician schedules, patient monitor feeds, and lab/radiology alerts into the messaging engine, enabling automatic message routing (e.g., paging the on-call hospitalist) based on real-time patient and staff circumstances, enhancing response times.
- Artificial Intelligence and Automation: AI/ML is increasingly used for clinical alerts. Vendors are creating AI chatbots and triage engines to evaluate alarms, prioritize severe events, and minimize alert fatigue. Natural-language processing and predictive analytics direct critical notifications to the appropriate caregivers.
- Wearables and IoT Integration: Wearable devices and Internet of Things (IoT) monitors, such as continuous vital sensors and portable telemetry, are integrated into CC&C platforms. Real-time vital sign data collected from bedside monitors or wearable patches can trigger alerts automatically and be sent through the communication system. This trend blurs the distinction between patient monitoring and clinical messaging.
- Cloud-Based and Open-API Systems: Many hospitals are moving CC&C to the cloud for scalability and mobile access. New solutions emphasize interoperability standards (FHIR, HL7, SMART on FHIR) and open APIs (promoted by the 21st Century Cures Act), enabling data flow between EHRs, CC&C apps, and patient smartphones. Vendor roadmaps increasingly highlight cloud-native architectures and partnerships (e.g., Cisco Webex Health Clouds, Microsoft Azure integrations).